Pelvic floor manual therapy is a specialized approach focusing on restoring strength and function to pelvic muscles through targeted techniques. It aims to address issues like pain, incontinence, and prolapse, enhancing overall pelvic health and quality of life.
1.1. What is Pelvic Floor Manual Therapy?
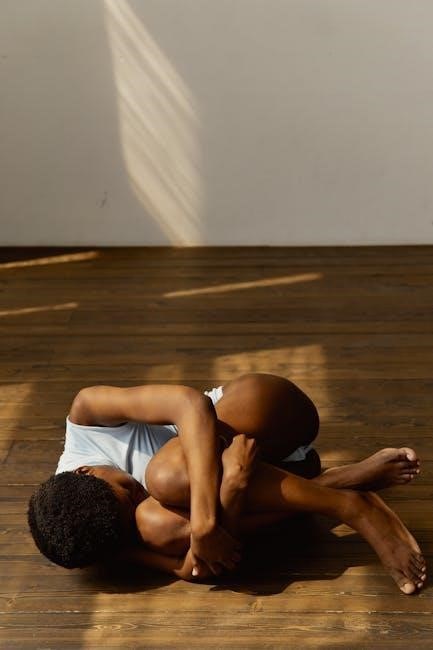
Pelvic floor manual therapy is a non-invasive, hands-on treatment approach designed to improve pelvic muscle function and overall pelvic health. It involves specialized techniques such as soft tissue massage, joint mobilization, and myofascial release to restore balance and strength to the pelvic floor muscles. Licensed physical therapists with expertise in pelvic health typically perform this therapy to address conditions like pelvic pain, incontinence, and prolapse. The therapy is tailored to individual needs, focusing on pain relief, muscle relaxation, and enhanced mobility. By targeting the root cause of dysfunction, it promotes long-term pelvic stability and improves quality of life for patients.
Anatomy of the Pelvic Floor
The pelvic floor consists of muscles, ligaments, and fascia supporting pelvic organs. Key structures include the levator ani, coccygeus, and pubococcygeus muscles, essential for bladder, bowel, and reproductive function.
2.1. Key Muscles and Structures
The pelvic floor is primarily composed of the levator ani, pubococcygeus, and iliococcygeus muscles, which form a supportive hammock for pelvic organs. These muscles work alongside ligaments and fascia to maintain pelvic stability. The pubococcygeus muscle plays a central role in bladder and bowel control, while the levator ani provides broader support. Ligaments, such as the pubovesical and uterosacral, further stabilize the bladder, uterus, and bowel. Together, these structures ensure proper organ positioning, facilitate reproduction, and enable continence. Dysfunction in these muscles or connective tissues can lead to pelvic floor-related issues, making them a focus in manual therapy interventions.

Conditions Treated with Pelvic Floor Manual Therapy
Pelvic floor manual therapy addresses various conditions, including pelvic floor dysfunction, chronic pelvic pain, urinary incontinence, and pelvic organ prolapse. These treatments aim to restore muscle function and stability.
3.1. Pelvic Floor Dysfunction

Pelvic floor dysfunction refers to a range of issues where the muscles and tissues of the pelvic floor fail to function properly. This can lead to symptoms such as pain, pressure, and difficulty with bladder, bowel, or sexual function. Common complaints include urinary urgency, constipation, and discomfort during intimacy. Pelvic floor manual therapy is often used to address these issues by restoring muscle strength and improving coordination. Techniques like soft tissue massage and myofascial release help alleviate tension and promote healing. By targeting the root cause of dysfunction, therapy can significantly improve quality of life and reduce symptoms associated with pelvic floor disorders.
3.2. Chronic Pelvic Pain
Chronic pelvic pain is a persistent and debilitating condition affecting millions, often linked to pelvic floor muscle tension or dysfunction. It can manifest as pain during urination, intercourse, or even during daily activities. Causes include musculoskeletal imbalances, scar tissue, or underlying conditions like endometriosis or interstitial cystitis. Pelvic floor manual therapy is highly effective in addressing this pain by releasing tight muscles, improving circulation, and restoring proper muscle function; Techniques such as myofascial release and joint mobilization help reduce inflammation and break pain cycles, offering long-term relief and improved quality of life for those suffering from chronic pelvic pain.
3.3. Urinary Incontinence
Urinary incontinence is a common condition characterized by involuntary loss of urine, often due to weakened pelvic floor muscles or nerve damage. Pelvic floor manual therapy plays a crucial role in addressing this issue by strengthening the muscles that support the bladder and urethra. Techniques such as soft tissue massage and myofascial release help improve muscle tone, enhance neural control, and restore proper bladder function. Regular therapy sessions can significantly reduce symptoms of incontinence, providing individuals with greater confidence and improved quality of life. It is a non-invasive and effective approach to managing this often debilitating condition.
3.4. Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the muscles and tissues supporting the pelvic organs weaken, causing these organs to drop out of their normal position. Pelvic floor manual therapy is an effective treatment approach, focusing on strengthening the pelvic floor muscles and improving their coordination. Techniques such as myofascial release and soft tissue massage help restore muscle tone, reducing symptoms like pelvic pressure and discomfort. By addressing the root cause of prolapse, manual therapy can enhance pelvic stability and improve quality of life for individuals experiencing this condition. It is a non-invasive and highly beneficial treatment option for managing prolapse symptoms.
Techniques Used in Pelvic Floor Manual Therapy
Pelvic floor manual therapy incorporates non-invasive, hands-on techniques to restore muscle function, reduce pain, and improve pelvic stability. These methods are tailored to address specific needs effectively.
4.1. Soft Tissue Massage
Soft tissue massage is a key technique in pelvic floor manual therapy, focusing on the manipulation of muscles, tendons, and connective tissues. It aims to relieve tension, reduce pain, and improve circulation. Gentle strokes and targeted pressure are applied to relax tight muscles, address spasms, and enhance flexibility. This method is particularly effective for individuals with chronic pelvic pain or muscle dysfunction; By promoting relaxation and reducing inflammation, soft tissue massage supports the restoration of normal pelvic floor function. It is often combined with other therapies, such as myofascial release, to create a comprehensive treatment plan tailored to individual needs.
4.2. Joint Mobilization
Joint mobilization is a technique used in pelvic floor manual therapy to improve joint mobility and reduce stiffness. It involves gentle, controlled movements applied to the sacroiliac, hip, or lumbar spine joints to restore normal function. This method helps alleviate pain and restricted movement, addressing issues like sacroiliac dysfunction or chronic pelvic pain. By enhancing joint flexibility and reducing muscle tension, joint mobilization supports overall pelvic stability. It is often combined with soft tissue massage or myofascial release for a comprehensive approach to treating pelvic floor disorders, promoting long-term relief and improved quality of life for patients.
4.3. Myofascial Release
Myofascial release is a gentle, non-invasive technique used in pelvic floor manual therapy to target the fascia, a connective tissue surrounding muscles and organs. By applying sustained, gentle pressure, therapists release tension and restrictions in the fascia, improving circulation and reducing pain. This method is particularly effective for addressing chronic pelvic pain, muscle spasms, and limited mobility; Myofascial release enhances the flexibility and elasticity of the pelvic floor fascia, promoting relaxation and restoring normal movement. It is often combined with other techniques, such as soft tissue massage, to provide comprehensive relief and improve overall pelvic floor function and comfort.

Benefits of Pelvic Floor Manual Therapy
Pelvic floor manual therapy enhances muscle strength, reduces pain, and improves pelvic stability. It restores function, alleviates symptoms like incontinence, and boosts overall pelvic health and well-being.
5.1. Improved Pelvic Muscle Strength
Pelvic floor manual therapy strengthens the pelvic muscles, improving their tone and resilience. Techniques like soft tissue massage and myofascial release target muscle imbalances, enhancing neuromuscular control. This leads to better bladder and bowel function, reducing incontinence and prolapse risks. Strengthening these muscles also supports pelvic organ stability, relieving pain during physical activity or intimacy. Over time, consistent therapy can restore muscle function, empowering individuals to maintain proper posture and movement patterns. Improved muscle strength fosters long-term pelvic health, reducing the need for surgical interventions and enhancing overall quality of life.
5.2. Reduced Pelvic Pain
Pelvic floor manual therapy is highly effective in reducing pelvic pain by addressing muscle tension and improving circulation. Techniques such as soft tissue massage and myofascial release target tight pelvic muscles, relieving discomfort. Joint mobilization enhances joint flexibility, reducing stiffness and pain. These therapies promote relaxation and restore normal muscle function, leading to significant pain relief. Over time, manual therapy can eliminate chronic pelvic pain, improving mobility and overall pelvic health. This non-invasive approach empowers individuals to manage pain without surgery, enhancing their quality of life and allowing them to engage in daily activities comfortably. Regular sessions often result in lasting pain reduction and improved well-being.
5.3. Enhanced Pelvic Stability
Pelvic floor manual therapy significantly enhances pelvic stability by strengthening the muscles and connective tissues that support the pelvic organs. Techniques like myofascial release and joint mobilization improve alignment and reduce strain on the pelvic structure. This therapy restores the natural balance of the pelvic floor, preventing excessive movement and instability. Enhanced stability reduces the risk of organ prolapse and improves posture, allowing for better distribution of force during physical activities. Over time, manual therapy fosters long-term pelvic health, enabling individuals to maintain proper alignment and enjoy improved mobility and confidence in their daily lives without discomfort or limitations.

When to Seek Pelvic Floor Manual Therapy
Seek pelvic floor manual therapy if experiencing chronic pain, incontinence, prolapse, or difficulty with bladder/bowel control. It’s also ideal for discomfort during intimacy or pelvic heaviness.
6.1. Signs and Symptoms Indicating the Need for Therapy
Individuals experiencing pelvic pain, urinary incontinence, or difficulty controlling bowel movements should consider pelvic floor manual therapy. Symptoms like pelvic organ prolapse, discomfort during intimacy, or a sensation of pelvic heaviness are key indicators. Additionally, those with chronic lower back pain or bladder/bowel control issues may benefit. Therapy is also recommended for postpartum women experiencing weakened pelvic muscles or new mothers facing incontinence or pain. Consulting a specialist is crucial if these symptoms persist or worsen over time, as early intervention can significantly improve pelvic health and overall well-being.
Finding a Qualified Pelvic Floor Manual Therapist
Look for a licensed physical therapist with specialized training in pelvic floor rehabilitation. Ensure they have certifications from reputable organizations and experience in treating pelvic health issues. Seek recommendations and reviews to find a qualified practitioner who can address your specific needs effectively.
7.1. Credentials and Specializations to Look For
When seeking a pelvic floor manual therapist, ensure they hold a license in physical therapy or a related field. Look for certifications like OCS (Orthopedic Clinical Specialist) or WCS (Women’s Health Clinical Specialist), which indicate advanced training in pelvic health. Membership in professional organizations, such as the American Physical Therapy Association (APTA) or the International Pelvic Pain Society (IPPS), demonstrates commitment to staying updated on evidence-based practices. Additionally, check for experience in treating pelvic floor conditions and positive patient reviews to confirm their expertise and effectiveness in addressing specific concerns.
Pelvic floor manual therapy is a crucial approach for improving pelvic health. It offers a safe and effective treatment for pain, incontinence, and prolapse, enhancing muscle strength and stability.
8.1. The Role of Pelvic Floor Manual Therapy in Pelvic Health
Pelvic floor manual therapy plays a vital role in restoring and maintaining pelvic health. It addresses conditions like pelvic floor dysfunction, chronic pain, incontinence, and prolapse through non-invasive techniques. By improving muscle strength, stability, and relaxation, it enhances overall pelvic function. This therapy is tailored to individual needs, offering a holistic approach to alleviate symptoms and improve quality of life. Its effectiveness lies in its ability to target the root cause of pelvic health issues, making it a valuable treatment option for those seeking relief and long-term wellness.
